22 April 2024
Early years packs developed at Oxford Brookes to be rolled out in Argentina
Innovative resource packs developed at Oxford Brookes University for families with babies and toddlers are to be distributed in Argentina.
Welcome to the Department of Psychology, Health and Professional Development, part of the Faculty of Health and Life Sciences. Our Department is a dynamic and diverse group of academics, researchers and professionals who are working collaboratively to better understand, and support, human development, health and well-being.
We offer a high-challenge, high-support environment, where you can work alongside our outstanding research and teaching staff, in order to develop your knowledge and skills, in research and professional practice, as well as take care of your post qualifying developmental needs.
The Department of Psychology, Health and Professional Development hosts a 'Flying Faculty' model, which currently is being delivered in both Hong Kong and Gibraltar. A ‘Flying Faculty’ model refers to academic provision that is accredited by Oxford Brookes University, and is delivered in international locations by Oxford Brookes Academic staff.

Research in the Department of Psychology, Health and Professional Development offers a supportive and collaborative research community, giving you the chance to develop your research skills together with knowledge of your chosen subject.
We pride ourselves on ensuring that our research and teaching is linked locally, nationally, and internationally, to our stakeholders and to the wider professional disciplines we represent. We have particularly strong links with local Trusts and Social Welfare organisations, both private, voluntary and independent, as well as statutory provisions.
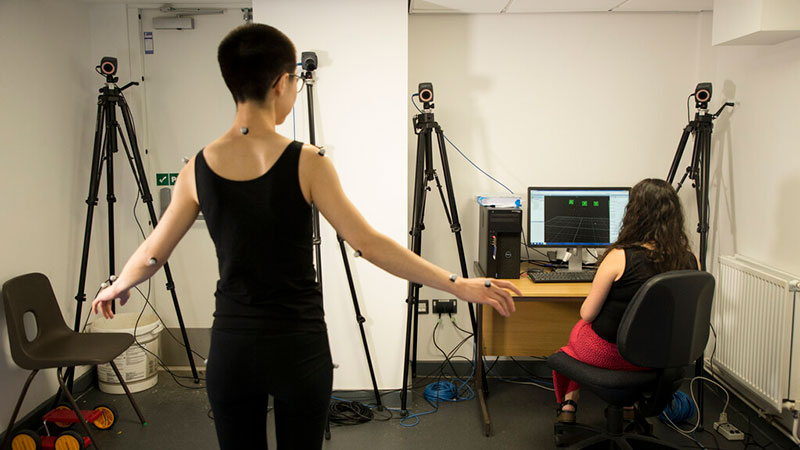
We offer a range of Psychology courses, designed to provide you with a solid grounding in empirical methods, theories and discoveries, located in a purpose-built discipline area at the heart of the University campus, featuring state-of-the-art facilities and laboratories. We also offer professionally recognised qualifications in Paramedic Science, enabling you to take your first steps towards undertaking a professional career in health care. We offer programmes designed to support those in Management and Leadership roles within health and social welfare, as well as those who want to mentor and teach others in a professional context.
After you achieve your academic and/or professional qualification, we can offer a wide range of opportunities to support your continuing research/professional development by providing post-qualifying and postgraduate courses.

Innovative resource packs developed at Oxford Brookes University for families with babies and toddlers are to be distributed in Argentina.

There is no ‘one size fits all’ approach to raising awareness of the link between alcohol and breast cancer and helping people cut down or give up drinking, a study at Oxford Brookes University has found.

Harry Wood and Aliya Abbasi are kick-starting their careers as the first medical simulation technician apprentices at Oxford Brookes University.

General practice patients say that they are not sufficiently warned about the possibility of developing dependence or withdrawal symptoms from some prescribed drugs, according to a recent study.